What is Reflux?
What causes reflux?
The contents of the stomach (e.g. acid, pepsin & bile) may escape the stomach and “reflux” into the esophagus, and even up into the airway.
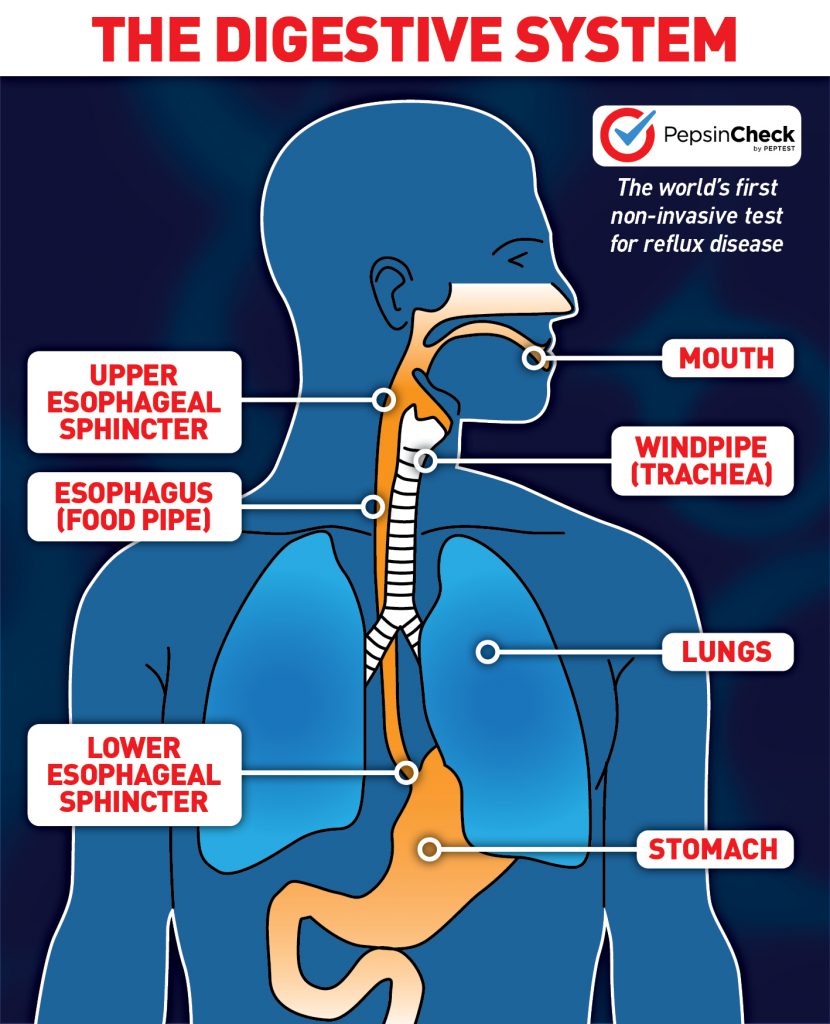
A ring of muscle called the lower esophageal sphincter (LES) connects the esophagus to the stomach. It opens to allow food to pass into the stomach and closes to prevent contents from flowing back into the oesophagus. When the LES is weak or damaged, it does not open and close properly. This malfunctioning allows stomach contents to travel the wrong direction, or reflux. When this occurs routinely, it is called gastroesophageal reflux disease (GERD).
During a reflux episode, stomach contents may reach beyond the upper esophageal sphincter (UES), a ring of muscle at the top of the esophagus. When reflux makes its way through the UES and into the throat, this is known as laryngopharyngeal reflux (LPR).
Reflux is often progressive -- the more someone refluxes, the more damage will be caused to the esophagus and airways which in turn will cause further reflux. Some people are genetically predisposed to reflux, but lifestyle and diet also play a large role in reflux symptoms. Over-eating, late-night eating, eating fatty foods, carbonated drinks, smoking, and alcohol can all trigger reflux. Anatomical and physiological factors also contribute to reflux disease; most commonly hiatal hernia, pregnancy, obesity, and sluggish digestion.
Symptoms of reflux
Gastroesophageal Reflux Disease (GERD) is associated with:
- Heartburn
- Difficulty with swallowing
- Nausea
- Inflammation of the oesophagus (oesophagitis)
- Regurgitation
- Occasional vomiting
Laryngopharyngeal Reflux is associated with:
- Sore throat
- Chronic cough
- A feeling of a lump in the throat
- Post nasal drip
- Persistent throat clearing
- Voice change
- Hoarseness
- Asthma
- Trouble swallowing
- Loss of dental enamel
What tests can indicate reflux?
If you have common symptoms of reflux disease, such as heartburn, regurgitation and difficulty swallowing, your physician may recommend a non-invasive preliminary test, such as PepsinCheck. A positive outcome may lead to medication and/or lifestyle advice, such as changing your dietary habits.
Medication can include over-the-counter antacids and prescribed proton-pump inhibitors (PPIs) or H2-receptor antagonists (H2RAs).
If symptoms are persistent, you may be advised to go for tests that aim to confirm or disprove the diagnosis of reflux disease – these are typically invasive diagnostic tests.
Reflux diagnosis typically entails several tests, such as 24/48 hour pH monitoring, impedance Testing, Barium Swallow, and Endoscopy, to establish whether reflux is the problem.
All expensive, invasive, time consuming and unpleasant for the patient.
How is reflux treated?
Following a positive reflux test your physician may suggest several treatment options depending on the severity of your condition and personal preference.
Treatment plans can include diet and lifestyle modifications, medication, therapeutic procedures, and surgery. Surgery is usually only recommended in cases of reflux disease that fail to respond to other treatments. Currently, Stretta Therapy is the only drugless, non-surgical procedure available. A physician applies Radiofrequency energy to the lower esophageal sphincter (LES) to strengthen the tissue and restore function.
Surgical procedures include:
- LINX Reflux Management System: a magnetic ring that is implanted to augment the LES functionality, intended to preserve normal physiologic function
- Medigus Ultrasonic Surgical Endostapler (MUSE) System, an endoscope device with a micro-camera, a surgical endostapler and an ultrasound sensor. It is used to wrap the top of the stomach around the lower end of the esophagus, reinforcing the closing function of the LES.
- Laparoscopic Nissen Fundoplication: this procedure involves wrapping the top section of the stomach around the esophagus, then it is stitched into place. The Nissen tightens the closing mechanism of the LES, creating a one-way valve to prevent stomach acid from refluxing into your oesophagus.
Is reflux dangerous?
A small amount of reflux is normal, but routine and severe reflux can lead to more serious complications, including Barrett’s esophagus, esophageal adenocarcinoma and potentially laryngeal cancer. If you have reflux symptoms, it’s very important to get evaluated and get your reflux under control. Like most diseases, early intervention is key!
